All About Plantar Fasciitis
On this page you can find informations about plantar fasciitis. Also you should visit our shoes for plantar fasciitis category for more information best protection for your feet
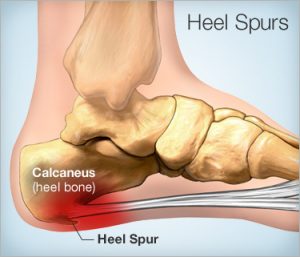
heel spurs_plantar fasciitis
Plantar fasciitis commonly causes stabbing pain that usually occurs with your first steps in the morning. As you get up and move more, the pain normally decreases, but it might return after long periods of standing or after rising from sitting.
Plantar fasciitis is more common in runners. In addition, people who are overweight and those who wear shoes with inadequate support have an increased risk of plantar fasciitis.
Age. Plantar fasciitis is most common between the ages of 40 and 60.
Certain types of exercise. Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballistic jumping activities, ballet dancing and aerobic dance — can contribute to an earlier onset of plantar fasciitis.
Foot mechanics. Being flat-footed, having a high arch or even having an abnormal pattern of walking can affect the way weight is distributed when you're standing and put added stress on the plantar fascia.
Obesity. Excess pounds put extra stress on your plantar fascia.
Occupations that keep you on your feet. Factory workers, teachers and others who spend most of their work hours walking or standing on hard surfaces can damage their plantar fascia.
- reflexes
- muscle tone
- sense of touch and sight
- coordination
- balance
An X-ray or an MRI scan may be necessary to check that nothing else is causing your heel pain, such as a bone fracture.
Reducing inflammation in the plantar fascia ligament is an important part of treatment, but this doesn’t address the underlying damage to the ligament.
Home treatments
Initial home treatment includes staying off your feet and applying ice for 15 to 20 minutes, three or four times per day to reduce swelling. You can also try reducing or changing your exercise activities. Using arch supports in your shoes and doing stretching exercises may also help to relieve pain. Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen (Motrin or Advil) and naproxen (Aleve), often reduce inflammation in the ligament.
Medical treatments
If home treatments and over-the-counter, anti-inflammatory drugs don’t ease the pain, an injection of a corticosteroid directly into the damaged section of the ligament can help. Your doctor can do this in their office. Your doctor may use an ultrasound device to help determine the best place for the injection. Your doctor can also apply corticosteroids to the skin of your heel or the arch of your foot, and then apply a painless electrical current to let the steroid pass through your skin and into the muscle. Physical therapy is an important part of treatment for plantar fasciitis. It can help stretch your plantar fascia and Achilles tendons. A physical therapist can also show you exercises to strengthen your lower leg muscles, helping to stabilize your walk and lessen the workload on your plantar fascia. If pain continues and other methods aren’t working, your doctor may recommend extracorporeal shock wave therapy. In this therapy, sound waves bombard your heel to stimulate healing within the ligament. Side effects of this treatment can include:
- bruises
- swelling
- pain
- numbness
Extracorporeal shock wave therapy hasn’t been proven to be consistently effective in relieving symptoms.
Surgery is the most dramatic therapy. This is done only in cases in which pain is severe. Your surgeon can partially detach the plantar fascia from the heel bone, but this weakens the arch of the foot and full function may be lost. Another surgery involves lengthening the calf muscle. This process is called gastrocnemius recession.
- legs
- knees
- hips
- back
Steroid injections and some other treatments can weaken the plantar fascia ligament and cause potential rupture of the ligament.
Surgery carries the risks of bleeding, infection, and reactions to anesthesia. Plantar fascia detachment can also cause changes in your foot and nerve damage. Gastrocnemius recession can also cause nerve damage.
- Your feet roll inward too much when you walk (excessive pronation).
- You have high arches or flat feet.
- You walk, stand, or run for long periods of time, especially on hard surfaces.
- You are overweight.
- You wear shoes that don't fit well or are worn out.
- You have tight Achilles tendons or calf muscles.
Stay with your treatment. If you don't, you may have constant pain when you stand or walk. The sooner you start treatment, the sooner your feet will stop hurting.